Lyme disease diagnosis
Lyme disease is diagnosed "typically made by recognition of the EM skin lesion; and or serologic testing to identify antibodies against B. burgdorferi antigens in patients with extra cutaneous manifestations of Lyme disease." The diagnosis of Lyme disease is mostly based on clinical features and is reinforced when the patient presents with an erythema migrans lesion and a history of residence or travel in an endemic area.
Patients often do not remember being bitten by a tick, but knowing if
they have had one in the past might be useful. Seroconversion might
happen late, not at all, or reflect a previous exposure rather than a
current infection, making serologic testing (like antibody titers)
frequently ambiguous and typical laboratory tests (like blood counts)
nonspecific for Lyme disease.
There are two stages to diagnose Lyme disease:
-
A clinical diagnosis is made based on the presence of an expanding, erythematous skin lesion measuring at least 5 cm in diameter and developing at the location of the tick bite. These lesions may emerge as targets or as homogenous lesions with central space. In patients with EM, antibodies are not consistently detected (<40% sensitivity). EM's differential diagnosis encompasses several skin disorders, including nummular eczema and tinea. Tick-associated rash illness (STARI) is one disease that may be clinically identical to another. It is an unidentified condition that also results from a tick bite, in this case, the bite of the Embryoma Americanum insect.
-
The serologic test. Serologic testing is the foundation of laboratory diagnosis for individuals with extra cutaneous Lyme disease symptoms. Seropositivity is sufficient to give a preliminary diagnosis when a patient exhibits apparent signs of extracutaneous Lyme disease. Two-step testing, as recommended by the current standards, often consists of an enzyme immunoassay (EIA) and a western blot test or tests to see if the EIA is reactive.
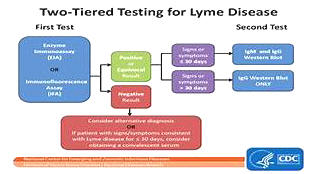
The majority of EIAs employ B. burgdorferi whole cell sonicate (WCS) as their antigen. Separate IgM and IgG western blot tests are advised as second-step testing for individuals with illnesses lasting more than four weeks with reactive first-step test results from EIA2. IgG western blot on its own is advised if symptoms have persisted for more than four weeks, as this test is sensitive to this kind of infection.
